 Patient non-compliance to treatment regimens has always been a significant challenge in chronic disease care. To quote an excerpt from a rather interesting MedScape CME education article, “Any drug that you do not take does not work” [1]. Patients' day-to-day decisions have a tremendous impact on the reported efficacy of treatment regimens and more importantly on their own health. Therefore, in the information age the favorable advocacy is for patients to be converted into active, informed participants taking ‘charge’ of their individual care management processes in order to guarantee the overarching success of the healthcare delivery system as a whole. Physicians must help patients take charge of their conditions by encouraging them to set self-management goals but also allow them to become actively involved with the diagnosis and selection of treatment options for their ailments. The old models of care where physicians would tell patients what to do and try to motivate them to change their habits or ways does not have a place in today’s day and age for a plethora of reasons which eventually boil down to fact that the average internet-enabled individual today does not like being told what to do without forming his / her own opinions. Working out a fool-proof way of getting through to the modern patient is one with substantial medical and economic ramifications. To shed some light on the substantial cost implications of effectively taking control of patient behavior, it is interesting to note that a majority of healthcare spending (outside of public-health expenditure) is affected by consumer choices. In fact, 69% of healthcare spending – including spending for catastrophic events attributed to chronic conditions, discretionary care and end-of-life care – is largely subject to individuals’ choices and behavior [2]. Assimilating the facts, therefore, informing patient behavior clearly has ramifications on both the effectiveness of patient care as well as healthcare economics. Now let us go over some interesting approaches which are gathering momentum in regard to informing patients about the state of their health and therefore indirectly allowing the healthcare system to begin gaining control of ‘patient behavior’. One way to make patients active participants in healthcare administration is to allow them to actively partake in the diagnosis of their health and further actually ‘operate’ diagnostic devices without scheduling appointments. This very concept is being pursued by a startup company from Ohio – HealthSpot [3], as well as Mayo Clinic [4] in the form of ‘diagnostic kiosks’ and is expected to make a revolutionary impact in regard to patient empowerment and reducing healthcare costs. Such technology has potential for impacting diagnosis and administration of treatments for minor and common health conditions such as the cold, earaches, sore throat, sinus infections, upper respiratory infections, rashes and skin conditions and eye conditions but tend to be less suited to management of ailments of less able-bodied patients with chronic conditions. Beyond the kiosk concept, several medical device startups – some with FDA 510k cleared product offerings – [5] as well as major technology firms such as Apple and Samsung are investing heavily in technology that can monitor a user's health using their mobile devices. As per a recent BBC News reported survey [6], more and more patients today are going to their general practitioner with preconceived notions regarding their expected treatment pathways which they glean based on information from apps and the internet. However, the BBC article also reports that often a patient's online diagnosis is not useful to the physicians. From the standpoint of the Devil’s Advocate to the above concepts, the hypothetical scenario of generating a population of non-medical trained but highly opinionated patient could be quite worrisome… In such a scenario, what might begin as a social issue of inappropriate self-administration of inordinate doses of over-the-counter medication may in the long term create a faction of quasi-trained healthcare professionals – or worse still, medical software / apps – with a greater power over patient beliefs than physicians themselves! So, how far must be actually go with regard the liberties offered to the active and informed patients in the care management process..? References: [1] “Adherence: The Silent CV Risk Factor” on Medscape. http://www.medscape.org/viewarticle/582903 [2] McKinsey International Survey on Healthcare’s Digital Future: http://www.mckinsey.com/insights/health_systems_and_services/healthcares_digital_future [3] HealthSpot: http://www.healthspot.net/ [4] Mayo Clinic Telehealth Kiosks: http://medcitynews.com/2014/10/mayo-clinic-telehealth-kiosks/ [5] http://medcitynews.com/2013/01/iphone-app-for-retinal-images-cleared-by-fda-could-expand-telemedicine-eye-exams-video/ [6] http://www.bbc.co.uk/news/technology-29458143 This blog entry is the result of playing chess against the computer on three long bus rides from the Faculty apartments in Shunde (China) to the location of the SYSU-CMU Joint Institute of Engineering (JIE) in Guangzhou (China). The hour long, bumpy bus rides were mind-numbingly boring with often very little breathing space, but they did offer me the opportunity to explore a game (viz. Chess) which I had long since forgotten about... Start: Shunde City, ChinaDestination: Sun Yat-sen University (SYSU) East Campus I never thought I'd miss driving a car so much - can't wait to get back home to Pittsburgh after this this semester of teaching at China ! Anyway... Back to Chess! The following are three interesting game-plays generated while playing against the computer (playing on the Chess.com iPhone app), each using similar opening strategies. The central theme behind the opening strategies employed in the following three games is 'The Ruy Lopez opening' for 'white'. This opening was invented sometime in the 1400's and has been proven to carry a small advantage to 'white'. This opening also allows for an early ability to 'castle' and build an attack. In games 1 and 3 below, I experiment with the Ruy Lopez opening as 'white' (each resulting in wins for 'white'), whereas in Game 2 I attempt the same opening and force a draw except this time playing as 'black'. In conclusion, it surely does seem like the Ruy Lopez opening is a promising one and can potentially provide either side (viz. 'white' or 'black') a marginal advantage; although, if you do end up playing against someone whom chooses this opening strategy it may certainly be possible to gain back the competitive edge with some tact! Game 1 - White (PGM) beats Black (Computer)Game 2 - Black (PGM) draws with White (Computer)Game 3 - White (PGM) beats Black (Computer) References:
1) www.Chess.com 2) http://www.chess.com/blog/monsterking/top-10-most-powerful-openings Acknowledgements: Special thanks to my wife, Jessika, for patiently reading the PGN Chess Codes to me which were essential to preparing this blog article. I also thank her and am grateful for her support in enduring this not-so-fun stint in China.  Image from http://www.itsmymedicare.org/ . Image from http://www.itsmymedicare.org/ . This post extends upon my previous blog entry on the 'waves' of healthcare IT adoption. The focus this time is on assimilating primary and secondary research in regard to ascertaining the optimal direction for new healthcare IT innovation and entrepreneurship initiatives, given the current healthcare climate... Healthcare IT adoption has been arguably most impactful in terms of enabling patient involvement in care management and accessibility to their digital health data through web-based or mobile applications. To successfully ride these trends of the third wave of healthcare IT adoption, healthcare companies need to follow the proven models of champions from the digital-service era like Google and Facebook by starting with a single focused end-user offering and then gradually add ergonomically designed conveniences which both keep the patient’s interests in mind and hold their attention, without introducing overt complexity. True empowerment in the digital era is about building value while ensuring comfortable interaction in a manner that necessitates negligible training (or none at all) to get acclimated to a new digital offering for patient enablement. In my last blog post we drew insights regarding what patients really want from digital healthcare through primary research [1]. But digital health systems around the world face challenges as well which is why any new patient enablement service offering needs to be positioned at the trade off of technical limitations on serviceability and scalability, and of-course patient needs. Limitations at the system level stem from the growing burden of chronic conditions which in-turn is a function of an aging population – 18% of the US population will be over 65 years old by 2025 – and the explosion of ‘lifestyle diseases’ relating to stress, mental illness etc.. But recall that over 70% of patients over 50 years old want digital healthcare services nearly as much as their younger counterparts for services such as finding and scheduling physician appointments [2] – therein stems the problem of scalability. While health promotion and prevention services are easy to advertise in a viral fashion through the digital media, managing prospective clientele and the resulting data from client-servicing has proven to be the technical bottleneck given that what patients really want in regard to better understanding the state of their health – as per primary research [1] – is fast availability of a personal contact person. Mushrooming hospital activity, unrelenting technological change, and costs of care rising at a rates faster than the general economy have reflected in increased financial wherewithal for the healthcare industry addition, while there remain concerns that the healthcare system is failing to meet the expectations that many people [3]. Common problems encountered by patients and ones that remain to be addressed by the healthcare IT revolution for patient enablement include reducing avoidable admissions and relieving the frustration that arises from long wait-times and having to repeat information and undergo repeat testing from a confusing array of healthcare professionals. The E-care digital revolution attempts to address these needs through the delivery of customer service via Internet-based user accounts, social networks and mobile applications, rather than call centers or service counters. E-care can significantly lower the cost of customer service operations [3] and despite their most obvious setback viz. the complete unavailability of a personal contact person, such digital services are in increasing demand by young, digitally enabled customers for whom online research and review of products is unremarkable. Assimilating the facts, especially given that the healthcare system is particularly failing in regard to servicing the needs of the elderly and those with chronic conditions while the use of mobile healthcare applications is strongest primarily among younger people, enabling services addressing the looming issues of healthcare accessibility via online platforms which include as much connectivity to ‘real people’ as possible seems to be the right direction for new healthcare IT innovation and entrepreneurship… References: [1] McKinsey International Survey on Healthcare’s Digital Future: http://www.mckinsey.com/insights/health_systems_and_services/healthcares_digital_future [2] Practo – the doctor search engine. www.practo.com [3] Why companies should care about e-care: http://www.mckinsey.com/insights/marketing_sales/why_companies_should_care_about_ecare?cid=DigitalEdge-eml-alt-mip-mck-oth-1408 Healthcare's Digital Future - Separating Myths from Realities uncovered from a McKinsey Survey7/13/2014  In earlier blog entries we have discussed specific avatars of Information Technology (IT) in the healthcare industry and touched upon how IT has been a driver of several megatrends. An interesting McKinsey publication from July 2014 [1] summarizing insights from a recent international survey highlights several key aspects of the healthcare industry wherein IT adoption has made a positive impact. The effect of IT has been reported to have occurred in a cascade of ‘waves’, occurring in chronological order, impacting:
In retrospect, granted our world is being revolutionized by technology driving healthcare digitization and advocating securely accessible data, how well have healthcare organizations been reading the signs in regard to patient-needs en-route to the goal of digital patient-enablement..? The McKinsey Digital Patient Survey conducted in 2014, in Germany, Singapore, and the United Kingdom, with a sample size greater than 1,000, reveals some surprising insights…
Riding the trends for the third wave of healthcare IT adoption, healthcare companies should follow the models of champions of the digital-service era like Google [3] and Facebook – start ‘small’ with a focused end-user offering and then continually add new services which both keep the customer’s (i.e. the patient) attention and build value, while ensuring the customer is comfortable interacting with the digital offering and requires little to no ‘patient enablement’ assistance to get acquainted with a new service. References: [1] McKinsey International Survey on Healthcare’s Digital Future: http://www.mckinsey.com/insights/health_systems_and_services/healthcares_digital_future [2] http://www.un.org/esa/population/publications/worldageing19502050/pdf/90chapteriv.pdf [3] Jeff Jarvis. What Would Google Do?, first edition, New York, NY: HarperCollins, 2009. Radiology Megatrends: Digitization, Quantification and Functionalization of Medical Imaging6/27/2014  Radiology information systems with picture archiving and communication capabilities have together provided modern radiology practices with the unlimited data storage and sharing capabilities necessary to cope with the ever-increasing routine data-demands. These systems offer patient-specific medical image management in a digitized format, according to the well-known standards elaborated in Digital Imaging and Communications in Medicine (DICOM) [1]. Digital image storage has potential to enable data access in a unified manner by departments even outside of the radiology department of a hospital provided server-side components and storage facilities are shared by all departments in the hospital. At the viewer’s end, digital systems can further be optimized for access by viewer computer systems (i.e. client systems) according to custom requirements of each clinical department in terms of resolution of rendering and image-processing capabilities. Image digitization has paved the way to effective structural visualization of diseased tissue or organs; today imaging has begun to have implications that transcend merely diagnostic value and is entering the realm of surgical planning minimally- or non-invasive examination and treatment through the realistic depiction of three-dimensional ‘depths’ of medical imaging as it relates to specific anatomical shapes. Image post-processing capabilities embedded in digital image management systems today often amplify the value of visualization by facilitating extraction of two or three dimensional measurements which is useful for purposes of reporting, and may employ cutting-edge digital signal processing technologies that quantify (or semi-quantify) either static or time-series image datasets. This augments the end-user’s cognitive capabilities by serving as a physician’s second-reader to accurately diagnose disease or plan out surgical decisions. Quantification of images has in-turn led into the concept of computer aided diagnostics (CAD), wherein a physician receives a diagnosis or ‘result’ from a non-human entity. CAD may be dubbed as ‘clinical intelligence’ to support daily radiology tasks and is often based on techniques employing machine-learning and data-based rule-learning technology which actually ‘arrive at’ a clinical decision rather than merely ‘guiding’ a physician towards one. This concept itself germinated in the 1960s but today has matured into a major focus of biomedical and clinical research relating to imaging-based biomarker discovery. Developments in this field of CAD have been incorporated into the routine diagnostic radiology approach to the structural screening of breast cancer on mammograms, early detection of heart disease [3-5] and even estimation of rupture risk of vascular aneurysms, to name just a few applications being investigated in this mushrooming space. But wait… there’s more! We can do even more with imaging today… One of the research domains receiving the most attention from funding agencies including the National Institutes of Health in the recent past has been the enabling of existing capital equipment with capabilities of imaging neuronal, cardiovascular and cellular ‘function’ as an extension to the convention of visualizing the structure of tissue or an organ. As opposed to structural imaging, functional imaging focuses on revealing physiological activities within a certain tissue or organ by employing medical image modalities that usually reflect a spatial distribution of injected tracers or probes within the body. Functional imaging has probably seen some of its greatest application in cognitive neuroimaging i.e. understanding the link between neuronal activity and functional imaging signals. A few functional imaging modalities which have made an impact in this space, to name a few, include positron emission tomography (PET), infrared imaging, Electroencephalography (EEG), Magnetoencephalography (MEG), functional magnetic resonance imaging (fMRI) [2] to detect blood-oxygen-level-dependent contrast material as an indicator of brain neuronal activity, and diffusion weighted imaging conducted by the Human Connectome Project which aims to understand the details of neural connectivity and build for the first time an integrated roadmap of structural as well as functional neural connections within the brain [3]… References: [1] DICOM. http://medical.nema.org/Dicom/ [2] Journal of Neuroscience Methods 74 (1997) 229–243. http://neurosci.info/courses/systems/FMRI/kim_fmri.pdf [3] http://www.humanconnectomeproject.org/about/  Megatrends are defined as global, sustained and macroeconomic forces of development that impact business, economy, society, cultures and personal lives, thereby defining our future world and its increasing pace of change. Three megatrends most relevant to medical imaging and radiology have been: a) Information Technology (IT) and Big Data; b) Demographic shifts defined by an ageing and growing population affecting healthcare expenditures; and c) Electronic, remote and mobile delivery of goods and services. Our first megatrend is a global trend seen across all industries and one that has affected each of our personal lives over the last 5 years –the need to collect large amounts of data. Be it photographs, documents, medical images or cloud services on our iPhones which justify never deleting another photograph to make space on our devices, the ‘big data’ megatrend has touched each of our lives. IT and the effective use of the same is an important cornerstone of the megatrends observable in the healthcare space today. Efficient management of vast amounts of rapidly generated data as well as management of clinical workflows is largely dependent on the development, accessibility and scalability of IT infrastructures supporting the healthcare industry. Our second megatrend relates to healthcare spending. 60% of a lifetime’s healthcare costs occur after the age of 65 years and by 2025 over 18% of the US population will be over 65 years old – an increase from 13% in 2010, amounting to an additional $4.5 trillion in healthcare spending! With an increased number of people spending time and money in hospitals, there is also a simultaneous growth in the number of deaths owing to medical errors – a whopping ~100,000 per year. Therefore, technologies for healthcare which present opportunities to save costs in terms of patient management while delivering optimal medical care with increased success rates and reduced rates of error are the ones which will define the healthcare delivery models of future. Such technologies will cumulatively shape tomorrow’s cost of another year of healthy life… The third megatrend of great relevance to healthcare is electronic delivery of goods and services in an era of rampant wireless device proliferation. Remote monitoring of patients and disruptive non-invasive diagnostic technologies are now ubiquitous while digital workflows such as teleradiology and distributed care which reduce costs and improve home healthcare efficiency as they allowing caregivers to manage time and resources more effectively. The ‘extended hospital’ today includes disruptive radiofrequency wireless-enabled technologies for remote diagnosis of cardiac health or injury and even telemonitoring technologies for monitoring patients over a wireless network, web video or the traditional telephones to reduce risk of death amongst critically ill or old patients while improving compliance in regard to medication regimens. Finally, to conclude on these megatrends and their affect on the healthcare practice, it is important to note that although technology revolution defined by these megatrends is ubiquitous, change is SLOW. Development and deployment of advanced IT-enabled goods and services in healthcare hasn’t enabled the same levels of transformation that have occurred in other industries for a number of reasons, the most important being the fact that healthcare is a brutally regulated space which is monopolized by a few omnipresent heavy-weights with the capital to surmount these regulatory hurdles. However, despite these shortcomings of technology adoption in healthcare and the unfairness of the competitive landscape, ‘healthcare IT’ is an umbrella for a host of technologies which together constitute the forefront of an overwhelming confluence of interests from stakeholders that range from the lay patient to physicians and business leaders. The digital, electronic and mobile technologies discussed in this post as well as several others breaking the threshold between academia and industry every day, will make a far-reaching financial impact that will disrupt the industry and drive real change in patient care, data management and healthcare-related business process workflows. References: * Images from http://suemontgomery.org/big-data-in-healthcare-collaboration-and-interoperability-are-essential-to-its-success/ , http://www.itpro.co.uk/strategy/20647/two-thirds-firms-will-invest-big-data-year-claims-gartner , http://blog.agfahealthcare.com/2013/06/11/the-icis-world-cloud/  Today I visited the Holocaust Museum, Yad Vashem, in Jerusalem, Israel. It was truly a frightening experience although the museum itself was a spectacular display of the carnage carried out by the Germans during Word War II (WWII). Revealing the truth about atrocities of WWII by sharing with us her grim experiences was Martha Weiss, holocaust death camp survivor, whom we were fortunate enough to meet as she reminisced the agony of what is meant to be a Holocaust Survivor... Martha was identified as being a Jew by a traitor in Holland where she had been safe for some years under the protection of a guardian and sent off with her elder sister to the Auschwitz Concentration Camp at age 8. Her parents had sent her to Holland, away her home in the Czechoslovakia, in order for her to remain in hiding under a false 'Aryan' identity and therefore avoid being snagged by anti-Semitic (and as it turns out, highly 'sadistic') German captors - the Nazi SS Officers - carrying out the bidding of Adolf Hitler whom we all know for his falsely justified virulent hatred of the Jews. As per some historians (and evidence in the museum) this false 'justification' for hating the Jews seems to have originated from Darwin’s original ‘survival of the fittest’ theory which was contorted into an incorrect understanding by Hitler’s administration - whom incidentally regarded themselves as 'intellectuals' - that developed and implemented policies designed to protect the ‘superior race’ (i.e. themselves, or as they termed themselves, 'Aryans') and simultaneously preventing the ‘inferior races’ (psychopathically inferred by Hitler and company as being those of Jewish faith) from mixing with those adjudged superior, in order to avoid 'contamination' of the latter’s gene pool [1]. What was originally planned as a mass exodus of those of Jewish faith from Germany, except for 'Essential Jews' whom were given a badge and made to work to support the genocide of their brethren, turn culminated in the ‘final solution’ for the extermination of approximately six million Jews when neighboring countries (as well as ones not so near by) to Germany refused to become 'involved'. In addition to the Jews, four million other people who belonged to what the German intelligentsia judged as ‘inferior races’ were also made to suffer, starve and then be murdered in cold blood. The brutal details of Martha's experiences are beyond the scope of this blog entry but several questions came to mind as I listened to her recounting the pathological and highly psychotic doings of the Nazi's in the pretext of 'Darwinism', and while I mental pieced together evidence presented along the museum's walls. Is being an anti-Semite a 'feature' encoded in the so called 'Aryan' DNA..? Is that why Hitler won his election to power with a landslide of 40% support from the German people..? Is this the reason the SS Officers in the concentration camps had the same virulent fervor as their monstrous and conceited leader - based on a vague theory of 'Darwinism'..? Is the anti-Semite pathology still latent in our DNA and is this why the world is still at war with the very victims of the holocaust ..? As I understand from recent visitors to Poland including the holocaust survivors, this virulent hatred for Jews is still rampant in the local population as is evidenced by conniving jives that roll off the tongues of ordinary people such as the conductors of trains as they pass by locations where concentration camps once murdered millions ( ... details available upon request). Could there be cure for this pathology in the interest of the human civilization being at peace with itself ..? The Yad Vashem museum provides us a glimpse of the what Jewish life had been before the War and unveils a brave image of the miserable life of slaves which the 'entire world' willed upon the Jews between the world wars and of-course the holocaust. Over 6 million were murdered but the museum has the goal of attributing a 'name' to every single victim of the holocaust whom were never given a righteous burial. Today they are at 4.2 million named victims and counting as historians continue to rummage through the remnants of the memoirs left behind by holocaust victims and their kin through whom they are survived today... References: [1] Darwinism and the Nazi Race Holocaust by Dr. Jerry Bergman on November 1, 1999. P.S - The following may be of interest: http://www.yadvashem.org/yv/en/newsletters/pdf/giving_030-032.pdf  A mere mile or so from the Gaza Strip, today I made an inspiring visit to a school with bomb-sheltered classrooms dedicated to education in social work (policy and law mostly). Their goal is improving the quality of life of the people in the community by 'listening' to them and helping them "access their rights". — at Sapir Academic College. This form of education is quite far removed from science and engineering but as far-reaching and impactful in my opinion as a life-saving surgical assist device or biomedical imaging technology. Such social work is what truly affects the changes for the good around us and it was a deeply touching experience to learn from the experiences of the numerous motivated social workers in Israel. Follow me on this story as well as the rest of my amazing journey through Israel, with the 2014 Faculty Fellows to Israel program (FF2Israel.org) on my FF2Israel webpage and of-course, on Facebook! 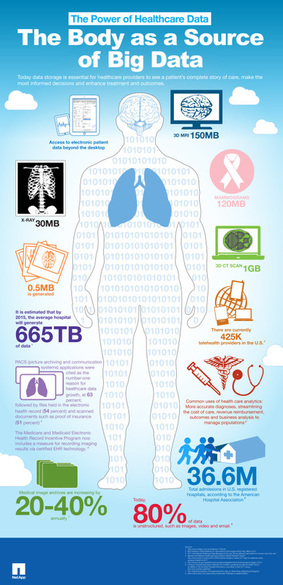 Radiology practices maintaining electronic patient records through digital radiology information systems (RIS) and vast amounts of imaging data through picture archiving and communication systems (PACS) are continuously faced with the problem of managing “big data”. The healthcare industry generates vast amounts of imaging data and therefore, PACS technology needs to keep up simply to cope with healthcare’s explosive production of data. An average hospital is expected to produce 665 Terabytes of medical data by 2015! These gargantuan and ever-increasing data requirements to store medical images and patient records have demanded the expansion of PACS storage capacities in orders of magnitude previously unfathomable in the print-radiology era. To gain some context in regard to the nature of this big data, let us try to visualize it. The infographic below [1], which was originally prepared by NetApp but which has since gained widespread popularity over the internet, provides an interesting quantitative perspective on the current scale as well as the projected scope of this “big data problem” that radiology practices in the healthcare industry faces today. Given these projections of data requirement growth rates, how must radiology practices act upon this knowledge today..? The right thoughts that should be running through the mind of a savvy healthcare IT professional are, “Should I be investing an inordinate amount of money in upfront capital investment on projected data storage capacities for the next decade, knowing only too well they will stay unused and idle during most of their lifetime..?” Further, notwithstanding the preeminence of tried and tested software available for recovery in the event of a data corruption or device malfunction incident, the unpredictable total costs of ownership over the lifetime of data, which incidentally encompasses maintenance, expansion, backup and replacement or recovery, is far from an alluring angle of owning and maintaining one’s own data-warehouse for medical images. What if it were possible to benefit from the digital age without having to belabor about shortcomings and unpredictable costs of ownership..? The solution is the cloud-based PACS which facilitates both data archiving and communication for remote access and retrieval of imaging data, entirely hosted in an off-site cloud server, managed and maintained by a HIPAA compliant third-party data-warehousing service provider i.e. the PACS vendor. While an end-user (client-side) installation of a traditional fully-equipped PACS system would involve a significant lead-time to set up and then an expensive end-user license agreement involving several annual (or multi-annual) scheduled maintenance updates, the cloud PACS services are usually plug-and-play services which are paid for on either an annual (and renewable) basis or a pay-per-patient (or per-access) service model. An important and highly valuable corollary of the fact that cloud-based systems require little to no time commitment from the customer for software or hardware maintenance activities, is that a cloud-based PACS always remains up-to-date as it is maintained by the PACS vendor! Another plus of a PACS-vendor on the cloud is the benefit of secure global access to your hospital data over an internet connection, behind the safeguards of robust protocols for authentication, authorization, and secrecy. To summarize, a new a cloud-based PACS can potentially offer your radiology practice better control and reliability in regard to imaging requirements outside of offering up huge saving in terms of unnecessary costs of owning and managing unwieldy data management equipment which eventually depreciate annually in terms of their asset value. So, if you’re struggling to keep up with your increasing patient data volumes, consider opting for the smart solution of a PACS-on-the-cloud which will seamlessly and effortlessly scale with your business and keep you at the helm of digital-imaging competitiveness, for absolutely no additional capital expense! References: [1] Big-Data infographic by NetApp: https://communities.netapp.com/docs/DOC-23102 . Also published in the blog of the Institute for health technology transformation,“The body as a source of big data.” Infographic Friday, March 15, 2013. Web: http://ihealthtran.com/wordpress/2013/03/infographic-friday-the-body-as-a-source-of-big-data/ . |
Personal thoughts on Imaging, IoT, Megatrends, Technology & Travel -
|
|
Copyright 2012-14, Prahlad G. Menon
|




 RSS Feed
RSS Feed
