Medical Imaging in a Digital Era - 14 July 2014
The electronic delivery of digital goods and services is omnipresent in today’s world where rampant wireless device proliferation and seemingly infinite cloud storage has pushed the boundaries of space as well as our imaginations ad infinitum. Be it photographs and documents hoarded via cloud services on our iPhones which justify never deleting another file, or medical images and health records of millions of patients generated and stored digitally by hospital systems worldwide, the ‘big data’ trend has touched each of our lives. The desperate need to collect large amounts of data has infected our world – but in some industries more than others… Information technology (IT) and the effective use of the same has been an important cornerstone of the megatrends observable in the healthcare industry today and the efficient management of vast amounts of rapidly generated data is shouldered upon the support of efficient and highly scalable IT infrastructures.
Gone are the days of inherently inefficient and unsustainable print radiology systems where images were prepared slowly and more often than not with substandard image quality. Digital data storage and retrieval has eliminated several steps in an otherwise convoluted print pipeline, paving the way for real-time reporting, on-the-fly quantitative analyses and minimal paper-pushing. In fact, an average hospital is expected to produce 665 Terabytes of medical data by 2015!
So, it is fair to say that radiology practices maintaining electronic patient records through digital radiology information systems and vast amounts of imaging data through picture archiving and communication systems (PACS) are continuously faced with the conundrum of managing big data. But this big data is doing a whole lot for the modern healthcare delivery model wherein electronic data access has for the first time presented the opportunity for patients to both understand the state of their health and participate in the care-giving process. Full digitization of the healthcare enterprise, including but not limited to electronic health records and digitization of medical imaging for radiology practices, has brought patient-care and patient-needs to the forefront of the care delivery mission.
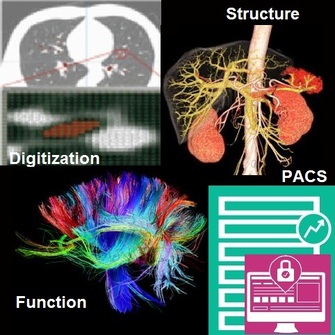
The manifestation of digitization and IT on specifically radiology image management has helped lower costs of healthcare practices the world over, while increasing efficiency and quality of reporting, therefore improving the overall sustainability and quality-of-care offered by modern radiology practices. Image digitization has simultaneously paved the way to quantitative structural and functional visualization of diseased tissue and organs which has in-turn begun to have implications that transcend merely diagnostic value and is entering the realm of surgical planning as well as guidance. Such quantification of medical images has further led into the concept of computer aided diagnostics (CAD), wherein a physician receives a diagnosis or ‘result’ from a computer algorithm suggesting solutions to complex and seemingly subjective questions such as screening for breast cancer on mammograms or even early detection of heart disease!
In summary, digitization and electronic delivery of healthcare data has not only augmented our ability to manage medical images but has paved the way to potentially improve the cognitive capabilities of clinical experts for the accurate diagnosis and effective management of disease or even surgical strategy. In future, medical imaging is likely to result in several far-reaching and impactful technical breakthroughs in fields ranging from neuronal signal processing and deciphering the relationship between brain structure and function, to forecasting the rupture risk of vascular aneurysms. So, stay tuned!
Gone are the days of inherently inefficient and unsustainable print radiology systems where images were prepared slowly and more often than not with substandard image quality. Digital data storage and retrieval has eliminated several steps in an otherwise convoluted print pipeline, paving the way for real-time reporting, on-the-fly quantitative analyses and minimal paper-pushing. In fact, an average hospital is expected to produce 665 Terabytes of medical data by 2015!
So, it is fair to say that radiology practices maintaining electronic patient records through digital radiology information systems and vast amounts of imaging data through picture archiving and communication systems (PACS) are continuously faced with the conundrum of managing big data. But this big data is doing a whole lot for the modern healthcare delivery model wherein electronic data access has for the first time presented the opportunity for patients to both understand the state of their health and participate in the care-giving process. Full digitization of the healthcare enterprise, including but not limited to electronic health records and digitization of medical imaging for radiology practices, has brought patient-care and patient-needs to the forefront of the care delivery mission.
The manifestation of digitization and IT on specifically radiology image management has helped lower costs of healthcare practices the world over, while increasing efficiency and quality of reporting, therefore improving the overall sustainability and quality-of-care offered by modern radiology practices. Image digitization has simultaneously paved the way to quantitative structural and functional visualization of diseased tissue and organs which has in-turn begun to have implications that transcend merely diagnostic value and is entering the realm of surgical planning as well as guidance. Such quantification of medical images has further led into the concept of computer aided diagnostics (CAD), wherein a physician receives a diagnosis or ‘result’ from a computer algorithm suggesting solutions to complex and seemingly subjective questions such as screening for breast cancer on mammograms or even early detection of heart disease!
In summary, digitization and electronic delivery of healthcare data has not only augmented our ability to manage medical images but has paved the way to potentially improve the cognitive capabilities of clinical experts for the accurate diagnosis and effective management of disease or even surgical strategy. In future, medical imaging is likely to result in several far-reaching and impactful technical breakthroughs in fields ranging from neuronal signal processing and deciphering the relationship between brain structure and function, to forecasting the rupture risk of vascular aneurysms. So, stay tuned!
Surviving in a Global Biomedical Research Community - 15 Feb 2013
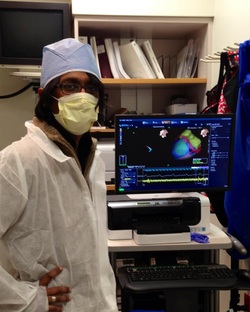
From diagnostics to surgical guidance, my mission is to use physics and computing to solve new, life-changing biomedical problems. Thanks to CMU’s ties to the Pittsburgh healthcare community, I’ve been recognized for doing this while still a graduate student. It all started with my being assigned to the cardiac MRI division of Allegheny General Hospital as part of the BME Clinical Practicum program. I chose to continue some cardiac MRI research that I’d begun on my own time with Drs. Mark Doyle, Robert Biederman and Steve Jones during the early months of my PhD. The research exposure offered me, invaluable experience in understanding the principles of biomedical research. .
During my time in Pittsburgh, I have conducted hands-on, supervised and unsupervised original research in two main areas: 1) cardiovascular biomechanics and 2) surgical planning for a range of minimally invasive and open-heart cardiac and vascular procedures. This has all been unpaid work outside of my PhD workload, done for the sole purpose of wanting to excel as a medical researcher. Some of this has translated into technologies that fuel my startup – a CMU-spinoff – QuantMD, LLC (www.quant.md)
The right way to strike a meaningful research relationship is to constitute mutually beneficial research goals in tandem with interested collaborators having the right resources at their disposal and similarly aligned ideals. Although student researchers often drive their projects, there exists a significant difference between the role of a student and that of a “PI” on a research project. As a student and innovator, my objective wasn’t to “raise money to solve a problem” but to simply ‘solve problems’ with few financial requirements or commitments – a distinct advantage for one motivated enough to prove their capabilities while contributing to relevant research problems addressed by scientific community.
The most important resource at my disposal and one that is perhaps the driving force behind all research endeavors has been ‘access to data’ – images from MRI, CT etc, or clinical data – across Pittsburgh. Data drives new insights into old problems and these new insights drive new technologies. Interested researchers, physicians, and supporters from industry can create a multitude of great opportunities – funding and in-kind support – to commercialize compelling technologies addressing social, clinical and technological needs in the clinic. In my experience, the result of successful collaborations in the Pittsburgh healthcare and entrepreneurial ecosystem, can help forge even stronger collaborations outside of the US – with burgeoning research communities in Europe, India, China.
While making every new connection count through one’s productivity is imperative, I find that successfully managing to imbibe and practice the ‘research culture’ is essential in order to facilitate compelling interest in indigenous novel research – this is the only way to secure a sustainable entrepreneurial future in the high-tech research community. The quintessential engineering research mindset is achieved not only by solid basic science fundamentals and technical prowess but also by strong conduct. Collaborating with a research group is for “you”, not for anyone else. While high impact research benefits everyone, including the researcher, it is a result of proactive ‘sharing’ of goals and motivations and more importantly a lot of ‘free public showcasing’ of work.
Finally, it is important to remember that as medical researchers affecting clinical practice we are accountable for results we produce as they will affect people’s lives. But as long as you’re aware of this and the responsibilities that come with it (J), employment of medical scientists is expected to increase at the rapid rate of 36% between 2010 and 2020, according to the bureau of labor statistics – well above the national averages for other professions! So, capitalize on all the in-kind support you can receive from the Pittsburgh medical community to actually make a difference in the science and rest assured, good work will not go unnoticed.
